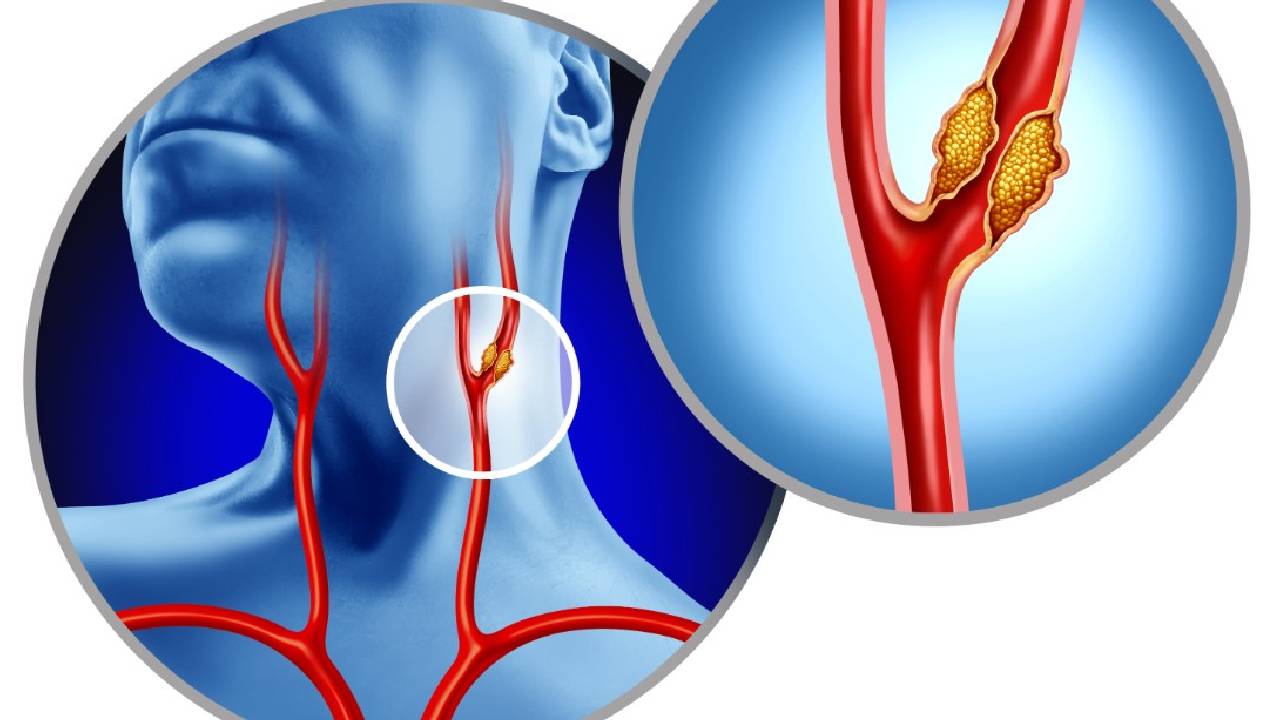
Carotid Revascularization
Definition:
Carotid revascularization is performed to treat carotid artery stenosis, typically caused by atherosclerosis, to reduce the risk of stroke.
Indications:
| Patient Type | Degree of Stenosis | Recommendation |
|---|---|---|
| Symptomatic (TIA/stroke) | ≥50% | Strong indication for revascularization |
| Asymptomatic | ≥70% | Consider in selected patients with low surgical risk |
Symptoms of Carotid Stenosis:
Transient ischemic attacks (TIAs)
Minor stroke
Sudden weakness, speech disturbance, or vision loss
Asymptomatic (detected via screening)
Diagnosis:
Carotid Duplex Ultrasound: Initial screening and surveillance tool
CT Angiography (CTA) / MR Angiography (MRA): Preoperative planning
Conventional Angiography: Gold standard (used selectively)
Treatment Options:
1. Carotid Endarterectomy (CEA):
Open surgical removal of atherosclerotic plaque.
Preferred in patients with low surgical risk.
Standard of care for symptomatic patients with high-grade stenosis.
2. Carotid Artery Stenting (CAS):
Minimally invasive approach via catheter.
Used for high surgical risk patients or those with prior neck surgery/radiation.
3. Best Medical Management:
Antiplatelet agents (aspirin, clopidogrel)
Statins
Blood pressure & diabetes control
Lifestyle modification (smoking cessation, diet, exercise)
Complications:
Stroke or TIA
Cranial nerve injury (more common in CEA)
Restenosis (re-narrowing of artery)
Bleeding or hematoma
Hyperperfusion syndrome
Follow-up:
Duplex ultrasound at 1, 6, and 12 months post-procedure
Lifelong risk factor control (BP, lipids, smoking)
Antiplatelet therapy continuation
Neurological monitoring